|
|

|
|
|
 |
 |
|
|
|
|
|
Eldercare
Can Be a Medical Deduction

With people living longer, many find themselves
becoming the care provider for elderly
parents, spouses and others who can no
longer live independently. When this happens,
questions always come up regarding the
tax ramifications associated with the
cost of nursing homes or in-home care.
Generally, the entire cost of nursing
homes, homes for the aged, and assisted
living facilities are deductible as a
medical expense, if the primary reason
for the individual being there is for
medical care or the individual is incapable
of self-care. This would include the entire
cost of meals and lodging at the facility.
On the other hand, if the individual is
in the facility primarily for personal
reasons, then only the expenses directly
related to medical care would be deductible
and the meals and lodging would not be
a deductible medical expense.
As an alternative to nursing homes, many
care providers are hiring day help or
live-in employees to provide the needed
care at home. When this is the case, the
services provided by the employees must
be allocated between household chores
and deductible nursing services. To be
deductible, the nursing services need
not be provided by a nurse so long as
the services are the same services that
would normally be provided by a nurse
such as administering medication, bathing,
feeding, dressing etc. If the employee
also provides general housekeeping services,
then the portion of employee's pay attributable
to household chores would not be a deductible
medical expense.
Household employees, like other employees,
are subject to Social Security and Medicare
taxes, and it is the responsibility of
the employer to withhold the employee's
share of these taxes and to pay the employer's
payroll taxes. Special rules for household
employees greatly simplify these payroll
withholding and reporting requirements
and allow the Federal payroll taxes to
be paid annually in conjunction with the
employer's individual 1040 tax return.
Federal income tax withholding is not
required unless both the employer and
the employee agree to withhold income
tax. However, the employer is still required
to issue a W-2 to the employee and file
the form with the Federal government.
A Federal Employer ID Number and a state
ID number must be obtained for reporting
purposes. Most states have special provisions
for reporting and paying state payroll
taxes on an annual basis that are similar
to the Federal reporting requirements.
If you need assistance in setting up a
household payroll, please contact this
office for additional details and filing
requirements.
|
|
|
|
Impairment-Related
Medical Expenses

Amounts paid for special equipment installed
in the home or for improvements may be
included in medical expenses, if their
main purpose is medical care for the taxpayer,
the spouse, or a dependent. The cost of
permanent improvements that increase the
value of the property may be partly included
as a medical expense. The cost of the
improvement is reduced by the increase
in the value of the property. The difference
is a medical expense. If the value of
the property is not increased by the improvement,
the entire cost is included as a medical
expense.
Certain improvements made to accommodate
a home to a taxpayer's disabled condition,
or that of the spouse or dependents who
live with the taxpayer, do not usually
increase the value of the home and the
cost can be included in full as medical
expenses. These improvements include,
but are not limited to, the following
items:
|
|
Constructing entrance or exit ramps
for the home,
|
|
|
Widening doorways at entrances
or exits to the home,
|
|
|
Widening or otherwise modifying
hallways and interior doorways,
|
|
|
Installing railings, support bars,
or other modifications,
|
|
|
Lowering or modifying kitchen cabinets
and equipment,
|
|
|
Moving or modifying electrical
outlets and fixtures,
|
|
|
Installing porch lifts and other
forms of lifts but generally not
elevators,
|
|
|
Modifying fire alarms, smoke detectors,
and other warning systems,
|
|
|
Modifying stairways,
|
|
|
Adding handrails or grab bars anywhere
(whether or not in bathrooms),
|
|
|
Modifying hardware on doors,
|
|
|
Modifying areas in front of entrance
and exit doorways, and
|
|
|
Grading the ground to provide access
to the residence.
Only reasonable costs to accommodate
a home to a disabled condition are
considered medical care. Additional
costs for personal motives, such
as for architectural or aesthetic
reasons, are not medical expenses.
|
|
|
|
|
Nursing
Services

Nursing Services Wages and other amounts
paid for nursing services can be included
in medical expenses. Services need not
be performed by a nurse as long as the
services are of a kind generally performed
by a nurse. This includes services connected
with caring for the patient's condition,
such as giving medication or changing
dressings, as well as bathing and grooming
the patient. These services can be provided
in the home or another care facility.
Generally, only the amount spent for nursing
services is a medical expense. If the
attendant also provides personal and household
services, these amounts must be divided
between the time spent performing household
and personal services and the time spent
for nursing services. However, certain
maintenance or personal care services
provided for qualified long-term care
can be included in medical expenses.
Additionally, certain expenses for household
services or for the care of a qualifying
individual incurred to allow the taxpayer
to work may qualify for the child and
dependent care credit. Part of the amounts
paid for that attendant's meals are also
included in medical expenses. Divide the
food expense among the household members
to find the cost of the attendant's food.
If additional amounts for household upkeep
were paid because of the attendant, include
the extra amounts with the medical expenses.
This includes extra rent or utilities
paid because a larger apartment was needed
to provide space for the attendant.
|
|
|
|
Medical
Dependents

Medical expenses paid for dependents may
be deducted. To claim these expenses,
the person must have been a dependent
either at the time the medical services
were provided or at the time the expenses
were paid. The qualifications for a medical
dependent are less stringent than those
for a regular dependent. A person generally
qualifies as a dependent for purposes
of the medical expense deduction if:
- That person
lived with the taxpayer for the entire
year as a member of the household or
is related
- That person
was a U.S. citizen or resident, or a
resident of Canada or Mexico for some
part of the calendar year in which the
tax year began, and
- The taxpayer
provided over half of that person's
total support for the calendar year.
Medical expenses of any person who is
a dependent may be included, even if
an exemption for him or her cannot be
claimed on the return.
Medical Expenses Under A
Multiple Support Agreement - Under
the provisions of a multiple support agreement,
only the one who is considered to have
provided more than half of a person's
support under such an agreement can deduct
medical expenses paid, but the medical
directly paid by that individual. Any
medical expenses paid by others who joined
in the agreement cannot be included as
medical expenses by anyone.
|
|
|
|
Support
Claimed Under a Multiple Support Agreement

A multiple support agreement is used when
two or more people provide more than half
of a person's support, but no one alone
provides more than half. Whoever is considered
to have provided more than half of a person's
support under such an agreement can deduct
medical expenses paid.
Any medical expenses paid by others who
joined in the agreement cannot be included
as medical expenses by anyone.
|
|
|
|
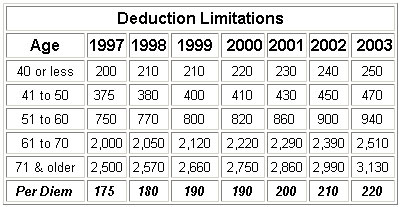
Long-Term
Care

Amounts paid for long-term care services
and certain premiums paid on long-term
care insurance are deductible as medical
expenses on Schedule A. Costs of care
provided by a relative who is not a licensed
professional or by a related corporation
or partnership don't qualify. The maximum
amount of long-term care premiums treated
as medical depends on the insured's age
and is inflation-indexed annually. The
following are the deductible amounts for
the past few years. If the taxpayer paid
long-term care premiums and qualifies
for a medical deduction on Schedule A
of their tax return and did not include
them in their medical deduction, the return
can be amended to include the deduction.
Please call this office to see if the
deduction will make a difference and to
have us prepare the amended returns.
Employees generally won't
be taxed on the value of coverage under
employer-provided long-term care plans.
However, the exclusion doesn't apply if
coverage is provided through a cafeteria
plan. In addition, long-term care services
can't be reimbursed tax-free under a flexible
spending account.
The "Long-term contract" is an
insurance contract that provides only
coverage of long-term care and meets certain
other requirements. Some long-term care
riders to life insurance will also qualify.
Benefits under a long-term care policy
after '96 (other than dividends or premium
refunds) are generally tax-free. For per-diem
contracts that pay a flat-rate benefit
without regard to actual long-term care
expenses incurred, the exclusion is limited
to $175 a day, indexed for medical cost
inflation (amount was $210 in 2002) except
when long-term care costs incurred are
more than the flat rate and are not otherwise
compensated by some other means.
A contract isn't treated as a qualified
long-term care contract unless the determination
of being chronically ill takes into account
at least five activities of daily living-eating,
toileting, transferring, bathing, dressing
and continence.
"Long-term care services" include
necessary diagnostic, preventive, therapeutic,
curing, treating, mitigating, and rehabilitative
services, maintenance or personal care
services prescribed by a licensed practitioner
for the chronically ill.
A "Chronically ill person" is one
who has been certified by a licensed healthcare
practitioner within the previous 12 months
as: (1) unable to perform at least two
activities of daily living (eating, toileting,
transferring, bathing, dressing, continence)
without substantial assistance for a period
of 90 days due to loss of functional capacity,
(2) having a similar level of disability
as determined in regulations, or (3) requiring
substantial supervision to protect from
threats to health and safety due to severe
cognitive impairment. The requirement
that a qualified long-term care insurance
contract must base its determination of
whether an individual is chronically ill
by taking into account five activities
of daily living applies only to (1) above
(being unable to perform at least two
activities of daily living).
|
|
|
|
Care
for the Elderly

When the elderly reach the point that
they can no longer care for themselves,
there are generally two courses of action
available to the caregiver; (1) Provide
for in-home care, or (2) place the individual
in a care facility. Each has its own distinct
tax ramifications:
|
|
In-home Care - If the elderly
person has the option to remain
in their home and provide in-home
care, that care is deductible as
a medical deduction, provided the
expenses are directly related to
the individual's medical care. If
the individual or individuals providing
that care also provide household
services, the cost must be allocated
between deductible medical expenses
and nondeductible personal expenses.
The individual or individuals providing
the care need not be a nurse, granted
they are providing services normally
administered by a nurse.
In-home care is also subject to
the rules for household employees
that require the employer (the elderly
individual) to withhold FICA and
Medicare taxes and issue a W-2 at
the end of the year. There are generally
state filing requirements as well,
so please call this office for assistance
in setting a household payroll.
|
|
|
Care Facility - If the option
is to place the elderly individual
in a care facility such as a convalescent
hospital, nursing home or a home
for the elderly, then the cost of
that care is deductible, provided
the primary reason for being there
is to receive medical care. If medical
care is the primary reason, then
the deduction will include the cost
of meals and lodging and no adjustment
is needed.
|
|
|
|
|
Medicaid
And Eldercare

Generally, after an individual has used
up all of their resources, Medicaid will
step in to provide the ongoing care of
the individual. Medicaid is usually a
combined Federal and state program that
pays for health and long-term care for
eligible low-income citizens and legal
residents of the United States.
It is not practical to explain all of
the various states programs. However,
since they are generally combined Federal
and state programs, there are similarities
among the various programs. This article
provides a brief overview of one state's
program. A Directory
of State sites allows you to review
the rules for any particular state.
California's version of Medicaid is referred
to as Medi-cal and the following is an
overview of the program's qualifications:
QUALIFYING FOR NURSING
HOME STAY - In order for Medi-Cal
to pay for a nursing home stay, the patient:
- Must be
admitted on a doctor's order,
- The stay
must be medically necessary, and
- With incomes
from any source are allowed to keep
only $35 per month for personal needs.
Patients with no income receive an SSI
grant of $40 per month for their Personal
Needs Allowance (PNA).
|
|
Patients who own their own home
- Medi-Cal recipients in nursing
homes who own their own homes (which
may be multiple dwelling units)
remain eligible for Medi-Cal as
long as:
- They
intend to return home; or
- The
residence is used by a spouse
and/or dependent relatives; or
- The
residence is used by a sibling
or adult child who lived there
at least one year before the owner
entered the nursing home; or
- They
make a good faith effort to sell
the home. Persons not capable
of making a good faith effort
to sell (for instance, those who
need conservatorships) remain
eligible for Medi-Cal. In that
case, bona fide steps have to
be taken so that someone else
can sell the home.
|
|
|
Married Couples - Couples
do not have to spend all their resources
in order for one spouse to be eligible
for Medi-Cal coverage in a nursing
facility. The person going into
the nursing facility can transfer
his or her interest in the home
to the spouse remaining at home
without affecting Medi-Cal eligibility.
A couple also may divide its non-exempt
property, so that the spouse at
home may keep up to $1,976 a month
of the couple's income and up to
$79,020 of the other assets for
his/her needs. The spouse at home
may also keep any independent income.
A couple may divide their property
however they wish. In determining
eligibility under the spousal impoverishment
provisions, Medi-Cal counts the
property held in the name of either
or both spouses. As soon as the
countable non-exempt property is
below $81,020 ($79,020 + $2,000
which can be retained by the institutionalized
spouse), the county can establish
initial eligibility. The couple
then has at least 90 days to transfer
everything but $2,000 into the name
of the non-institutionalized spouse.
The non-institutionalized spouse
may retain all of the income that
he or she receives in his or her
own name. Consult legal services
or a private attorney familiar with
Medi-Cal law if either you or your
spouse may need nursing facility
care.
|
FINANCING NURSING HOME CARE -
Generally, a nursing facility's administration
will help determine if the patient is
eligible for Medi-Cal to pay the costs
of the nursing home. If not, they can
explain under what conditions the patient
may become eligible in the future. The
law requires that nursing home residents
receive identical treatment regarding
transfer, discharge, and provision of
services regardless of the source of payment.
A Medi-Cal resident can stay in any bed
in a nursing facility.
Spousal Impoverishment Provision
- Couples looking at nursing home placement
for a spouse need to be aware of the special
laws enacted that allow the spouse remaining
at home to keep a certain amount of income
and resources when the other spouse enters
a nursing home. This is intended to prevent
impoverishment of the spouse at home.
|
|
Community spouse's monthly maintenance
needs allowance: The spouse
at home may keep all of the couple's
income up to $2,019 per month (this
is the base 1998 amount which is
adjusted annually for inflation).
This is called the community spouse's
"monthly maintenance needs allowance".
Note: This amount is adjusted annually
by a cost of living increase. The
spouse at home may obtain additional
income or resources through a "fair
hearing", or by court order.
If the spouse at home receives income
above the limit in his/her name
only, he/she can keep it all (this
is called the "name on the instrument
rule"); however, he/she will
not be allowed to keep any of the
nursing facility spouse's income.
Income received by the nursing facility
spouse will go to his/her share
of cost. The spouse in the nursing
home is allowed to keep $35 monthly
for personal needs ("personal needs
allowance").
|
|
|
Resources: The spouse at
home can keep up to $80,760 (this
is the base 1998 amount which is
adjusted annually for inflation)
in resources, and the institutionalized
spouse may keep up to $2,000. (Different
laws apply to spouses who entered
a nursing facility before September
30, 1989. If this is the case, the
individual should contact a lawyer/advocate
knowledgeable about this area of
the law.) Both separate property
(i.e., from a previous marriage
or inheritance) and community property
that is not exempt are combined
and counted at the time of application
for Medi-Cal. Once the resource
limit has been reached, all ownership
interest should be transferred to
the spouse at home. The institutionalized
spouse's $2,000 resource limit should
be kept separately and accounted
for separately.
|
TRANSFER OF ASSETS - Institutionalized
Medi-Cal recipients or applicants who
transfer non-exempt assets for less than
fair market value during a 36-month "look
back" period may be subject to a period
of ineligibility. The length of the ineligibility
period depends on the value of the transferred
asset or resource and date of transfer
period. The period of ineligibility begins
on the date the transfer was made. The
36-month "look back" period begins when
an institutionalized person applies for
Medi-Cal or when a Medi-Cal recipient
is admitted to a nursing facility. A 60-month
"look back" period for assets from certain
trusts is also required. Federal law amended
trust regulations makes it more difficult
to set up a Medicaid qualifying trust
for eligibility and estate claims purposes.
For a trust already established, it is
recommended that an attorney review it.
|
| |
| |
| |
|
|
|
|
|